1. From Diagnosis to Destiny: Diabetes doesn’t limit dreams.
A diabetes diagnosis is not the end of your goals.
With proper care, most people with diabetes can study, work, run businesses, have families, and live full lives.
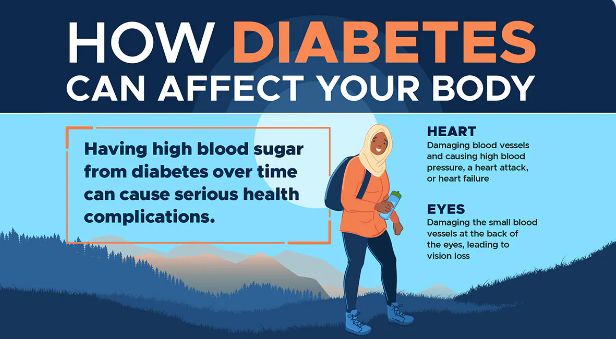
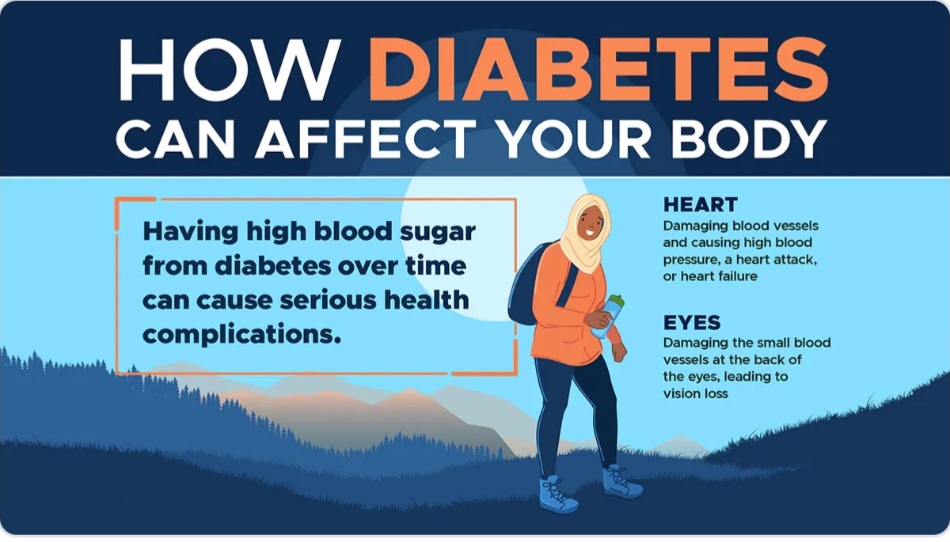
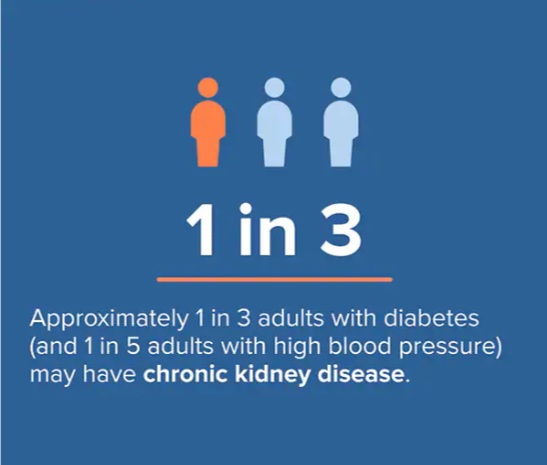
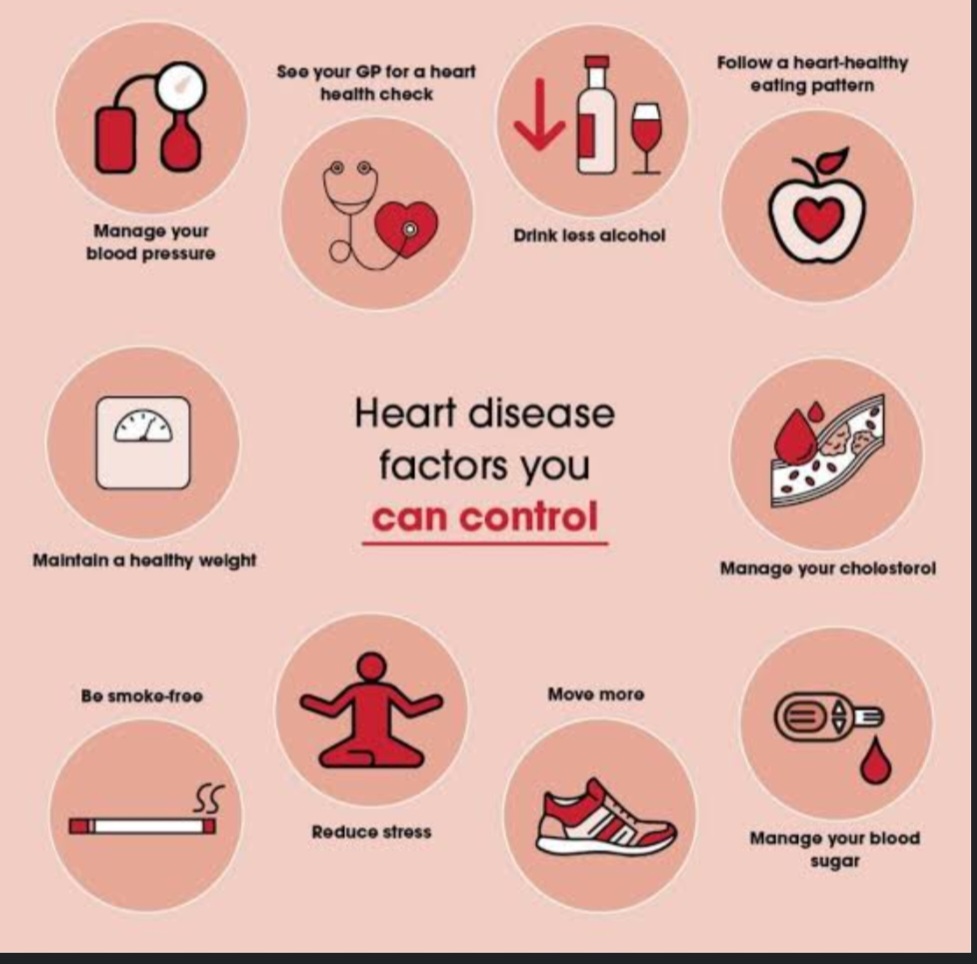
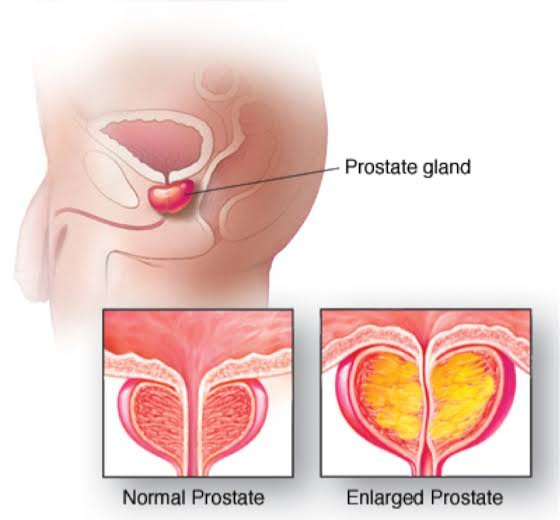
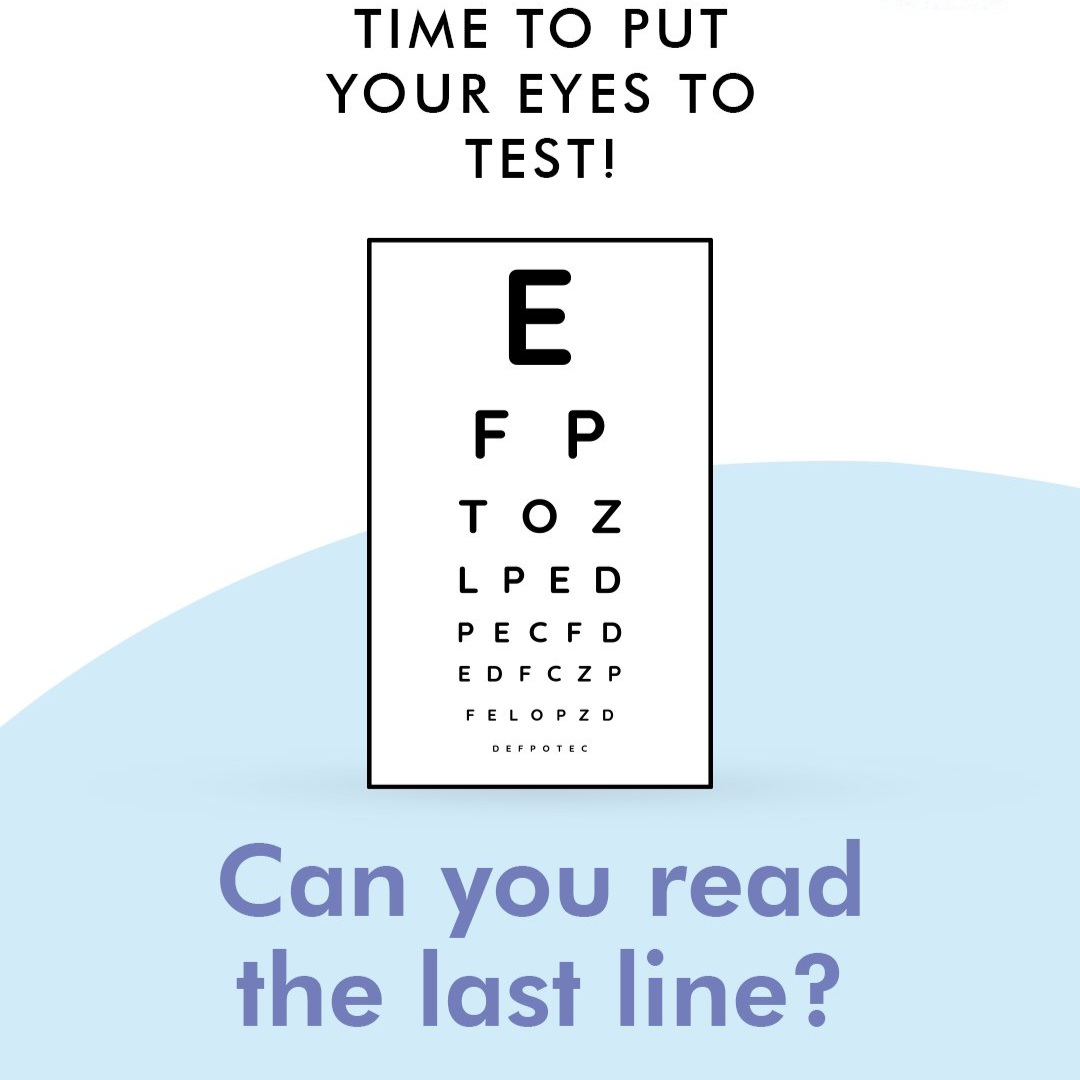
Good blood sugar control greatly reduces the risk of complications like kidney disease, eye disease, and heart problems.
What to do:
- Follow your treatment plan (insulin or tablets) as prescribed.
- Work with your healthcare provider to set realistic targets for blood sugar, blood pressure, and cholesterol.
- Set life goals (career, fitness, family) and plan how diabetes care fits into your routine, not the other way round.
Know your numbers & own your journey.
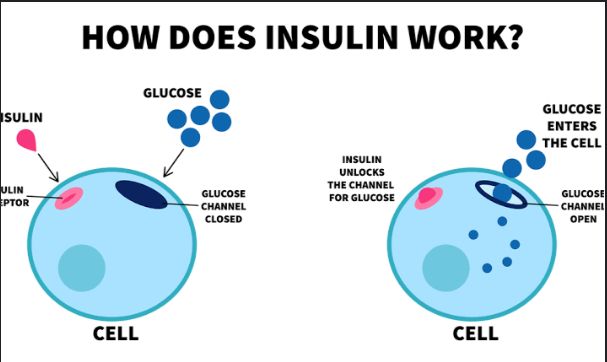
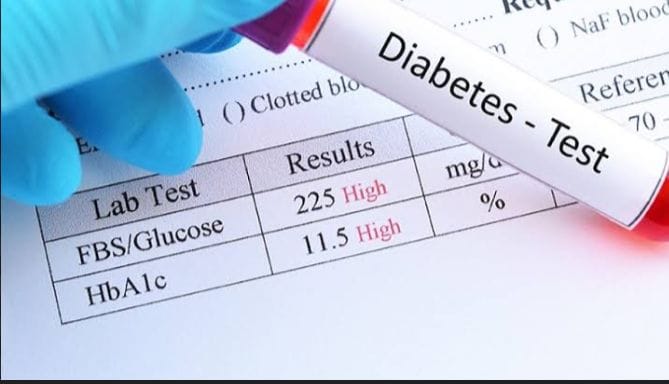
Understanding your blood sugar readings (fasting, random, HbA1c) helps you make daily decisions on food, activity, and medication.
What to do:
- Ask your provider: “What should my fasting sugar, random sugar, and HbA1c be?”
- Keep a small notebook or app log of readings and how you felt (e.g., “felt dizzy”, “ate late”, “skipped meal”).
- Bring this log to clinic visits – it helps personalize your care.
2. A Journey of Innovation & Hope: Treatment keeps getting better
Use today’s tools to your advantage.
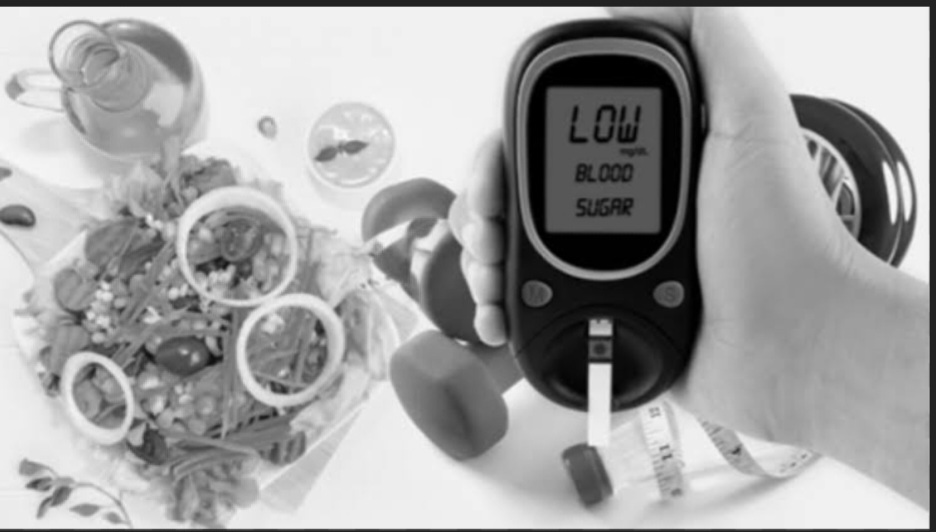
Modern diabetes care includes home glucose meters, continuous glucose monitors (CGMs), insulin pens/pumps, and digital apps. These tools help you monitor and adjust early before complications set in.
What to do:
- If you can, get a home glucose meter and learn how to use it correctly (wash hands, use fresh strips, note time and value).
- Ask your provider if CGMs, insulin pens, or apps are suitable and affordable for you.
- Even simple tech like SMS reminders or alarms on your phone can help you remember medicines and clinic appointments.
Regular follow-up is part of modern care.
Advances in diabetes treatment work best when combined with regular review. Clinics and telemedicine platforms (like Medicall Space) can adjust treatment early and prevent emergencies.
What to do:
- Keep routine checkups (usually every 3–6 months, or as advised).
- Use teleconsultations for early questions instead of waiting until you are very sick.
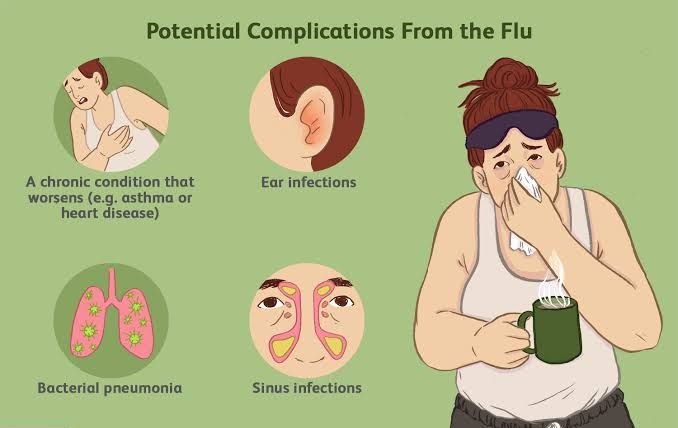
- Update your doctor if you start new medicines, herbal remedies, or notice new symptoms (numbness, blurred vision, swelling, chest pain).
3. Support Turns Challenges into Strength: You’re not alone
Involve your support system.
Family, friends, caregivers, and community groups can help you with daily routines and emotional support, which improves adherence and quality of life.
What to do (for people living with diabetes):
- Share basic info with a trusted person: what to do if your sugar is low (give fast sugar like juice, soda, glucose) or high (seek care, check dose).
- Teach close family how to recognize hypoglycaemia signs: sweating, shaking, confusion, fast heartbeat.
- Join a support group (local clinic, church group, WhatsApp group led by health professionals).
What to do (for family & caregivers):
- Encourage healthy eating at home so the person with diabetes isn’t isolated.
- Remind, don’t shame. Use phrases like, “How can I support you with your medicine today?” instead of blame.
- Accompany them to clinic occasionally to understand their care plan.
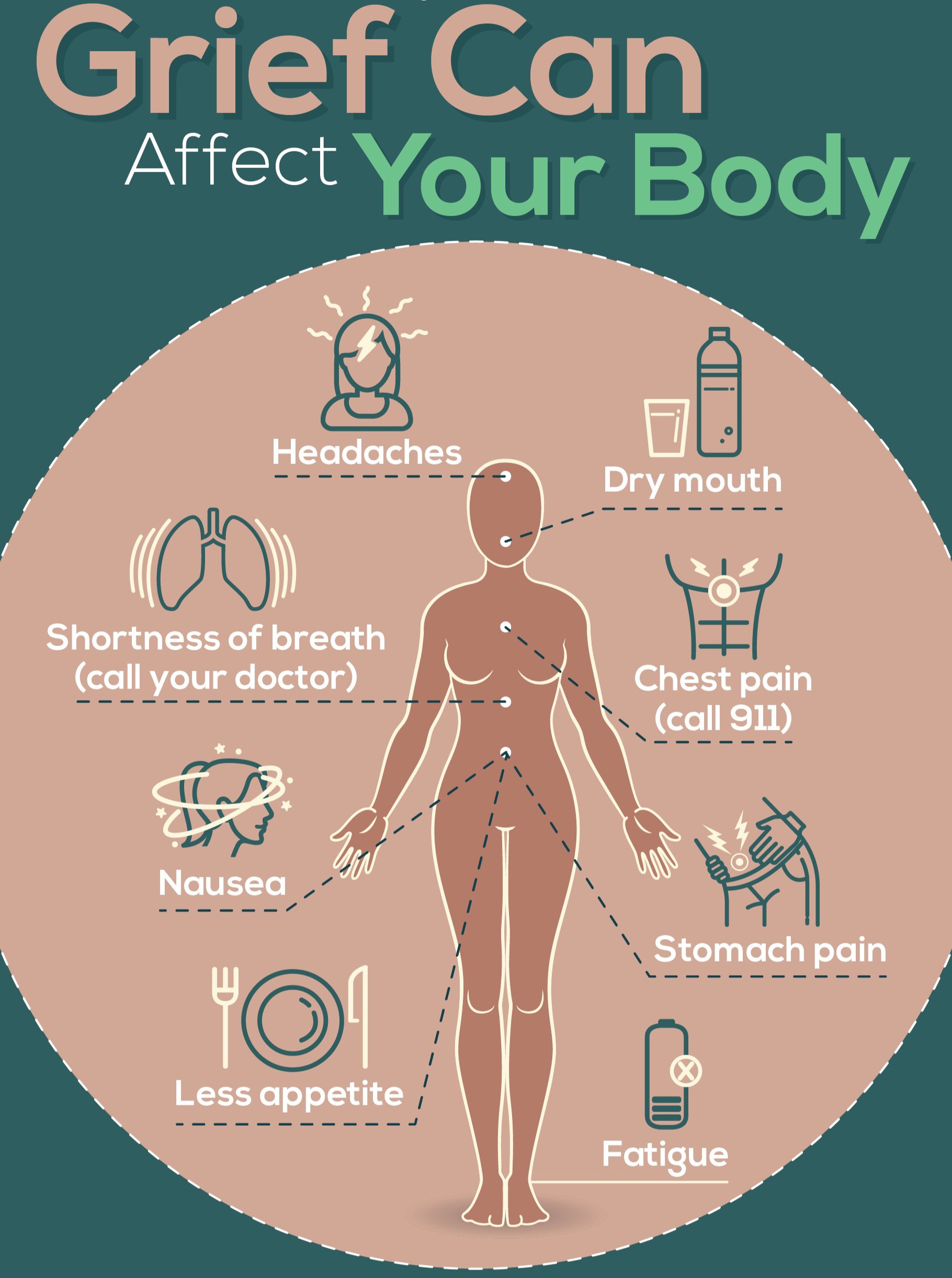
Mental health matters in diabetes care.
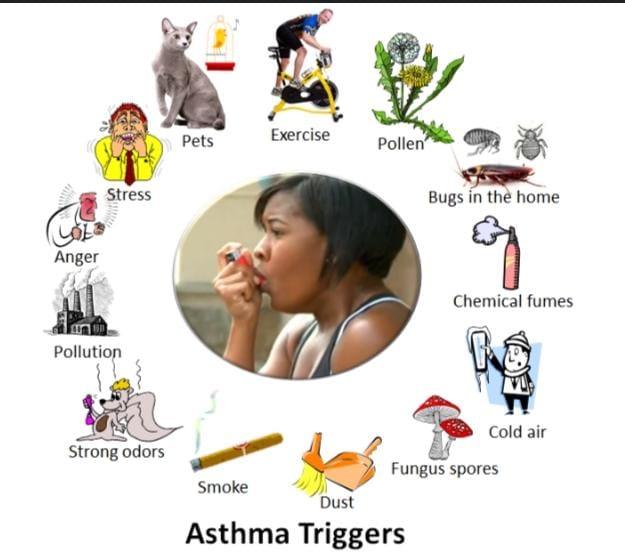
Living with a chronic condition can cause stress, anxiety, or depression, which can worsen sugar control.
What to do:
- Notice signs of burnout: feeling tired of measuring sugars, skipping meds, hopelessness.
- Talk openly with a healthcare provider or counsellor if you feel overwhelmed.
- Practice simple stress-management habits: deep breathing, short walks, prayer/meditation, journaling, safe social activities.
4. Live Well. Live Fully. Live Empowered: Everyday habits that protect your future
Build a simple daily routine.Stable daily habits help keep blood sugar more predictable.
Daily checklist idea:
- Food: Eat regular meals; avoid skipping then overeating later.
- Focus on:More vegetables and high-fibre carbs (whole grains, traditional foods in reasonable portions).
- Less sugary drinks and refined snacks.
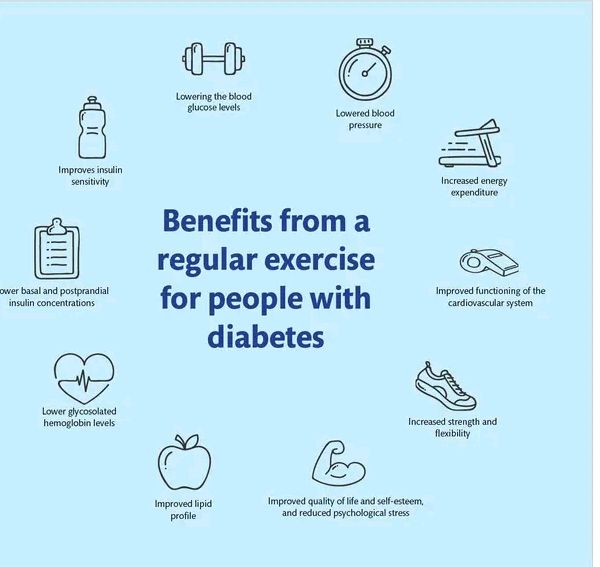
- Movement: Aim for at least 30 minutes of moderate activity (brisk walking, dancing, light jogging) on most days of the week, as allowed by your doctor.
- Medication: Take insulin/tablets at the correct time and dose.
Don’t skip checkups, even when you feel okay.
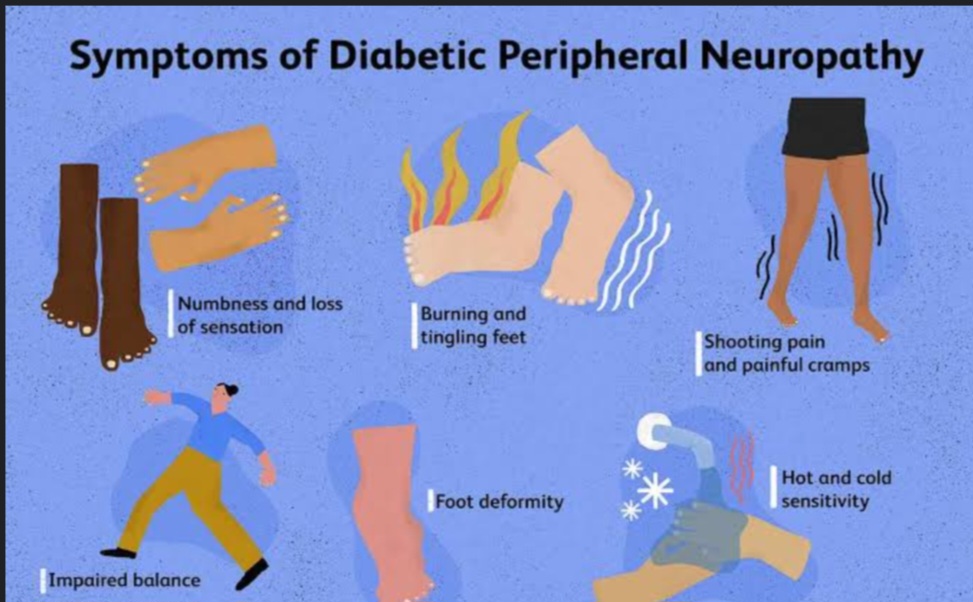
Complications often develop silently (especially eye, kidney, and nerve damage).
What to do:
- Schedule:Eye exam at least once a year.Kidney tests (urine and blood) as recommended.Foot checks (by you daily; by a provider at visits).
- Inspect your feet every day: look for cuts, blisters, colour changes, or lack of feeling.
- Wear comfortable shoes and avoid walking barefoot, especially outdoors.
Celebrate small wins- Improving diabetes control is a step-by-step process, not perfection.
5. We Celebrate Progress – and the Future: Hope + Prevention
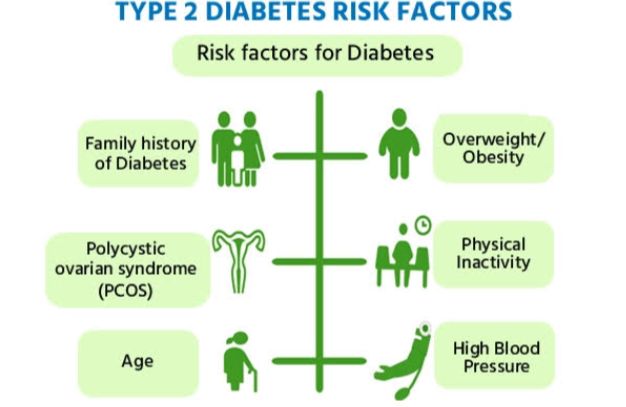
Prevent Type 2 diabetes where possible.
Many people are at risk (overweight, family history, high blood pressure, history of gestational diabetes, sedentary lifestyle). Lifestyle changes can delay or prevent type 2 diabetes in many cases.
What to do if you’re at risk:
- Get a screening test (fasting blood sugar, HbA1c) especially if:
- You are over 35–40 years.
- You have a close relative with diabetes.
- You are overweight/obese or have high blood pressure.
- Aim for gradual, sustainable weight loss if overweight (even 5–7% loss of body weight can reduce risk).
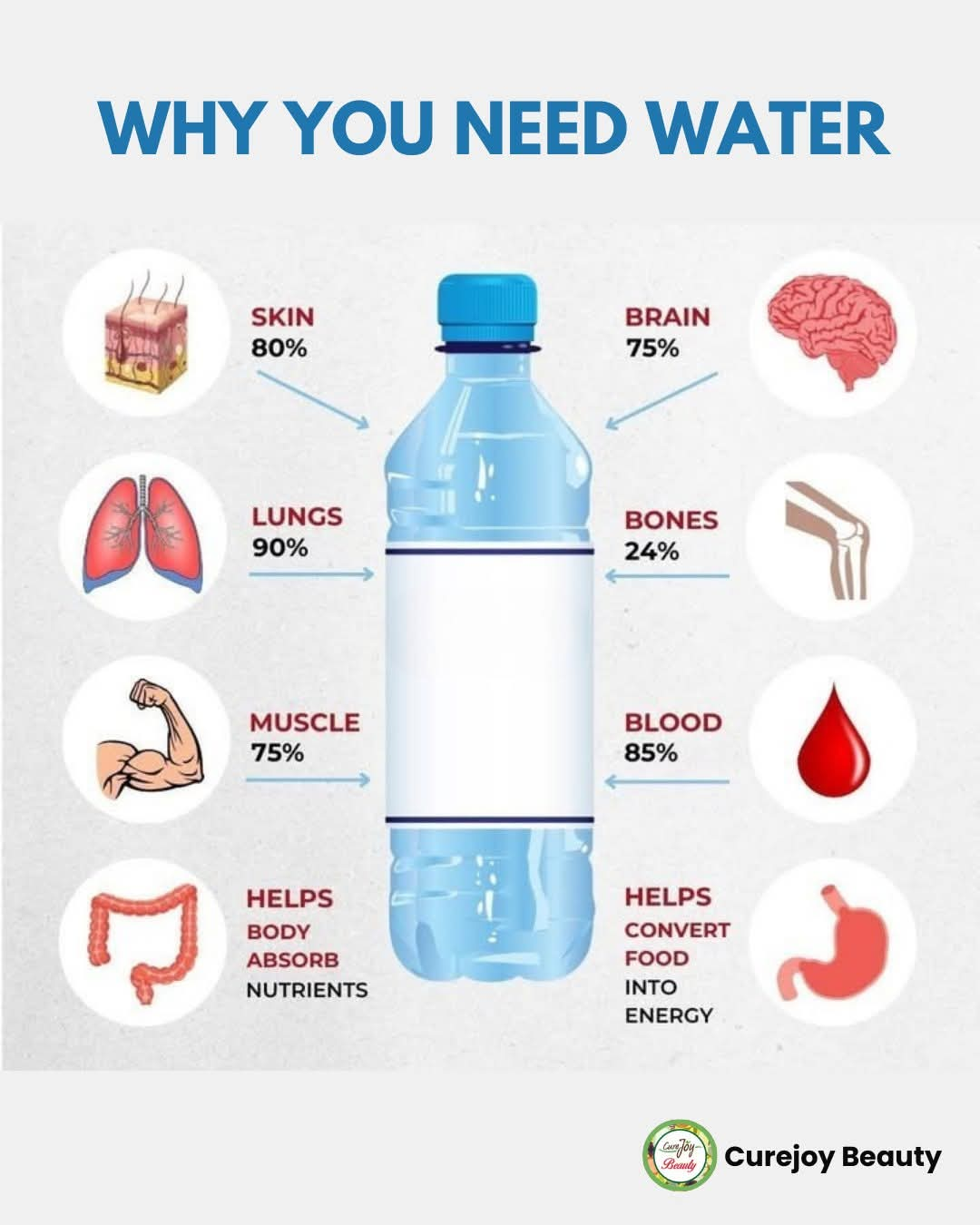
- Replace sugary drinks with water, and add more vegetables and whole grains to meals.
Know when to seek urgent help: Quick action can save life in diabetes emergencies.
Seek urgent care if:
- You have very high sugars with symptoms such as extreme thirst, frequent urination, abdominal pain, vomiting, deep breathing, confusion, fruity breath.
- You have signs of severe low sugar: confusion, inability to swallow, seizures, or loss of consciousness (someone nearby should give fast sugar if possible and rush you to hospital).
- You have chest pain, sudden weakness on one side, trouble speaking, or sudden vision loss, heart attack or stroke.