From Checklists to Clean Hands: Practical Guidance for Health Professionals
- Why Patient Safety Matters
According to the WHO, unsafe care is among the top 10 causes of death and disability worldwide, with up to 1 in 10 patients harmed in hospital settings. Preventable infections, medication errors, and communication failures cost millions of lives annually. Safe care reduces harm, improves patient trust, and is essential to high-quality healthcare.
Ensuring safety requires vigilance at every step of the patient journey.
- Patient Safety Guide Across the Care Journey
1. First Contact & Admission
Confirm Identity and Information. Verify patient identity (name, date of birth, ID number) at every stage of admission.
Accurate Documentation (CDC): Record complete medical history, allergies, and current medications to guide safe care.
Triage and Prioritization: Ensure patients in critical condition are identified and attended promptly to prevent avoidable deterioration.
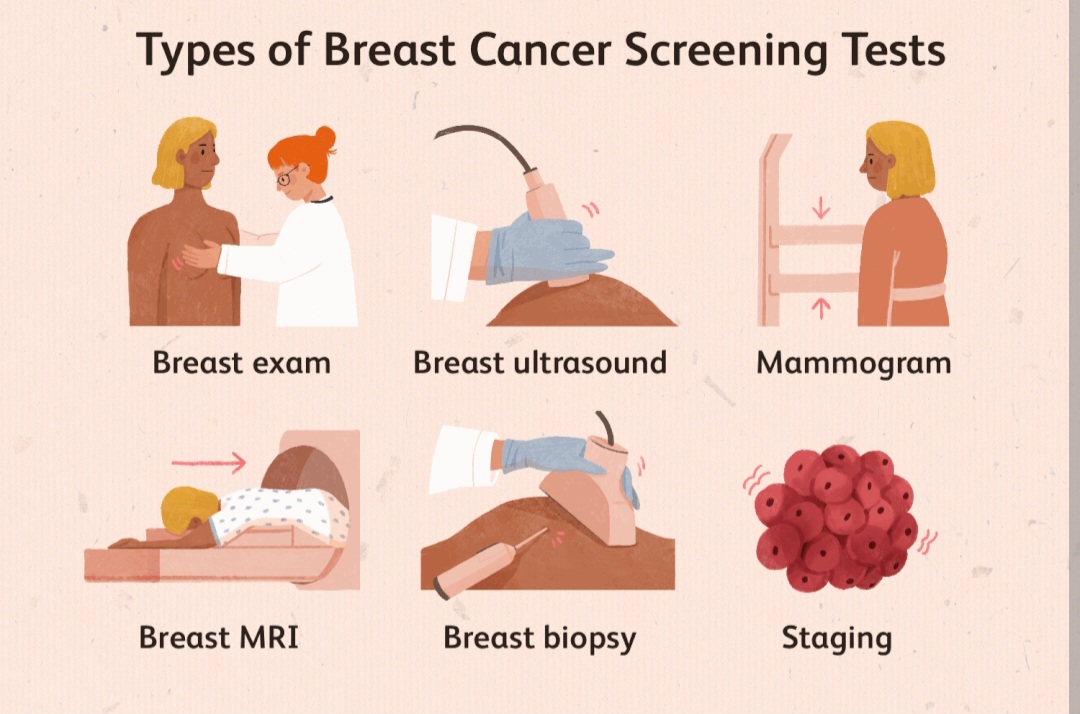
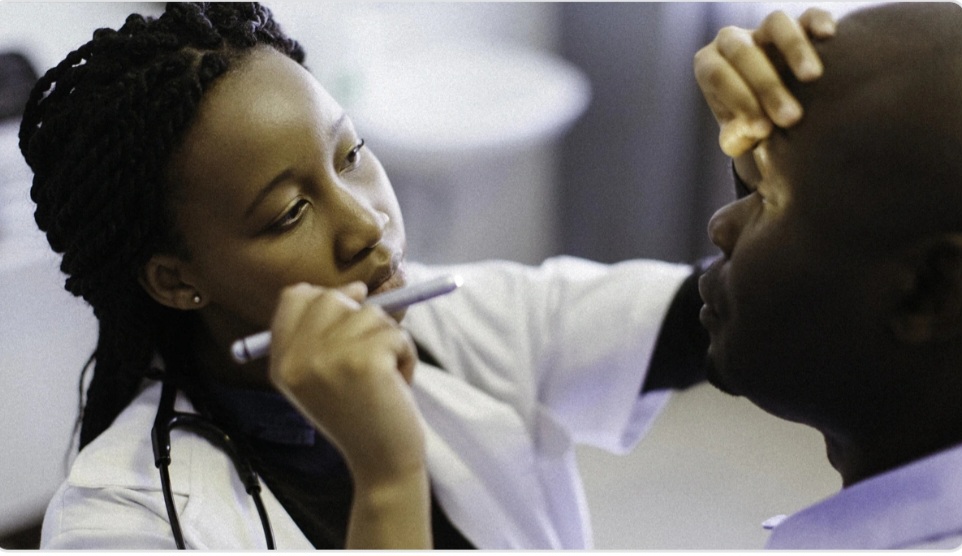
2. Diagnosis and Assessment
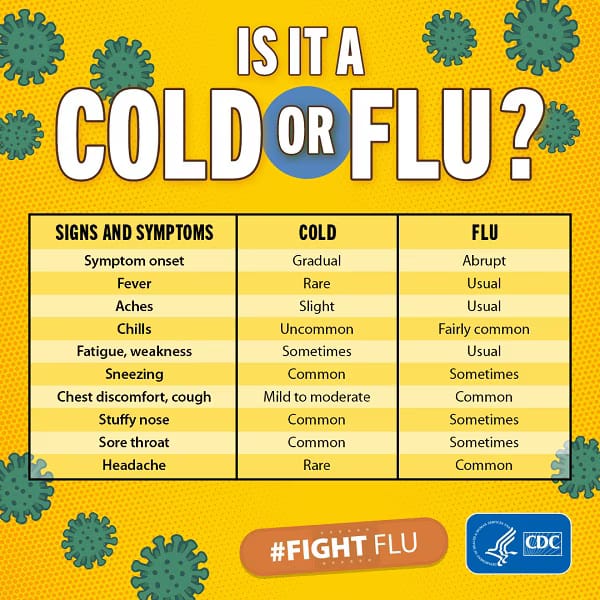
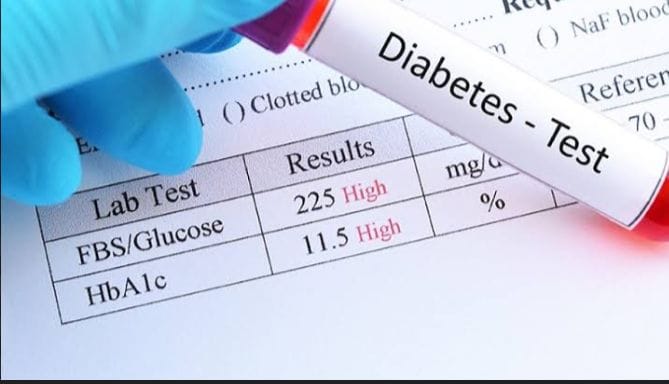
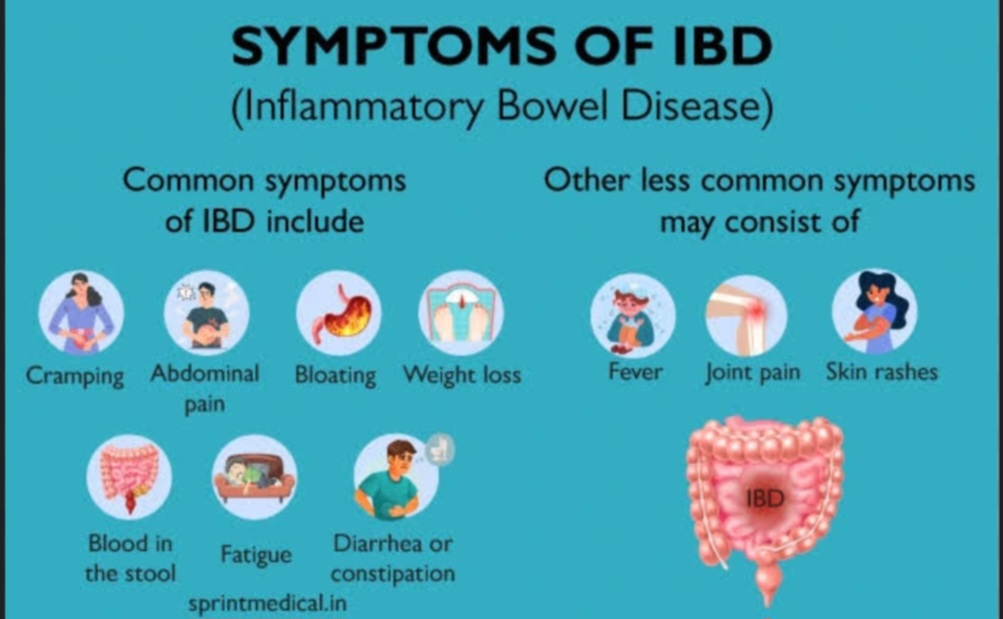
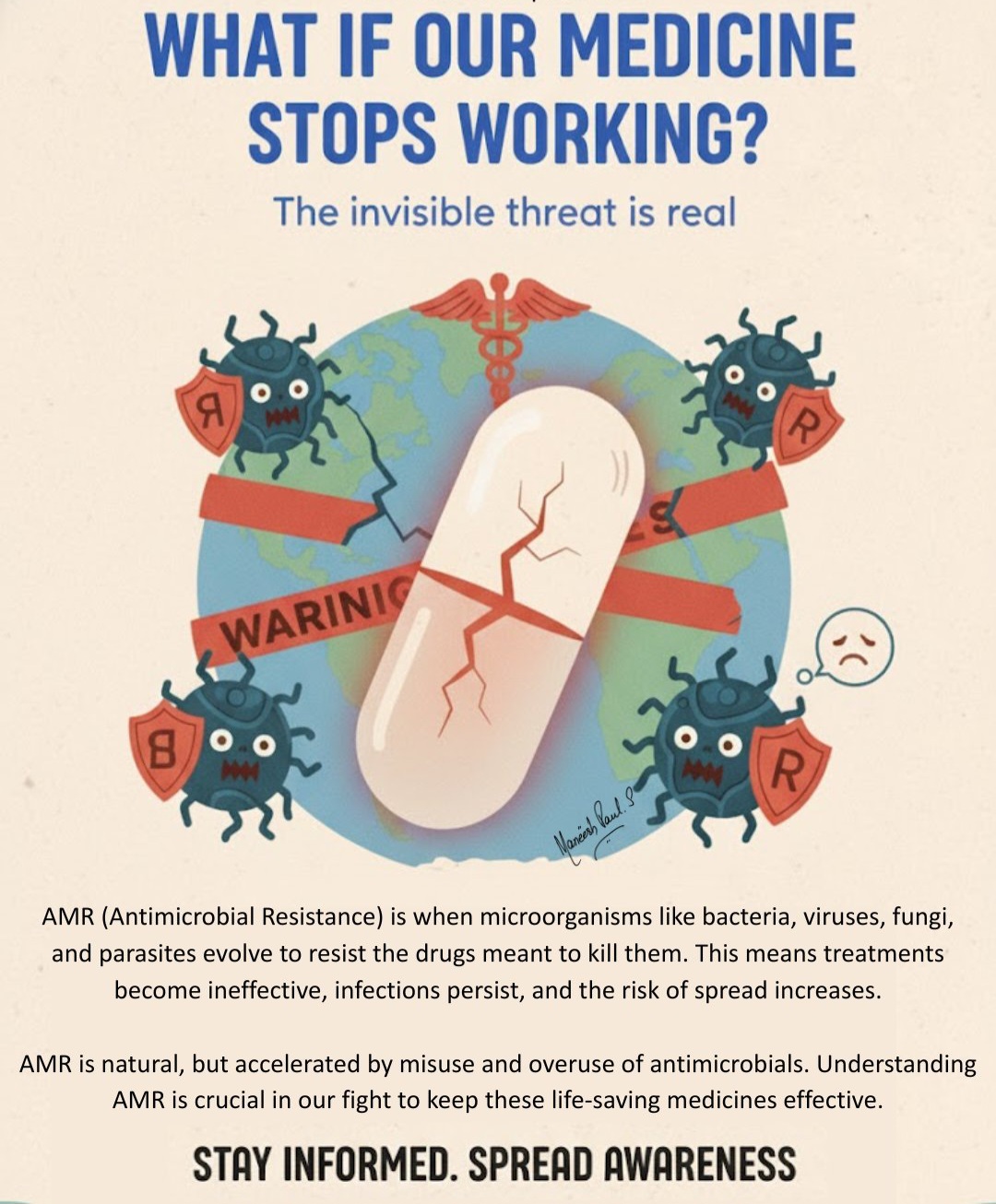
Avoid Misdiagnosis: Use evidence-based diagnostic tools and, where possible, a second opinion for complex cases.
Effective Communication : Discuss findings clearly with the care team and patient to avoid misunderstandings.
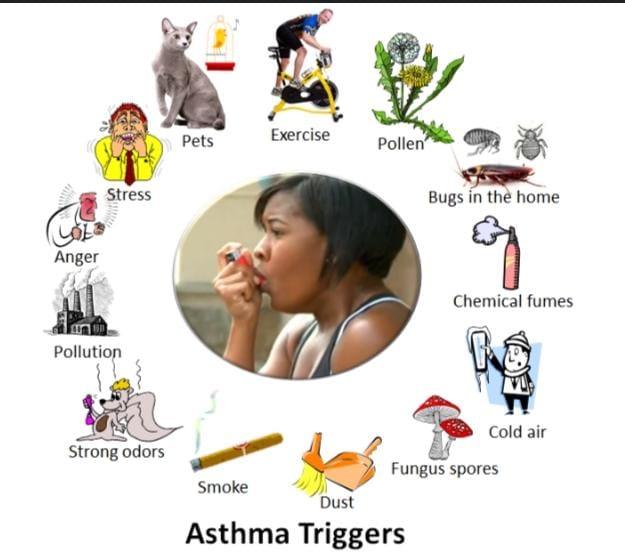
Respectful Engagement: Involve patients and families in discussing concerns and symptoms—they often provide vital safety clues.
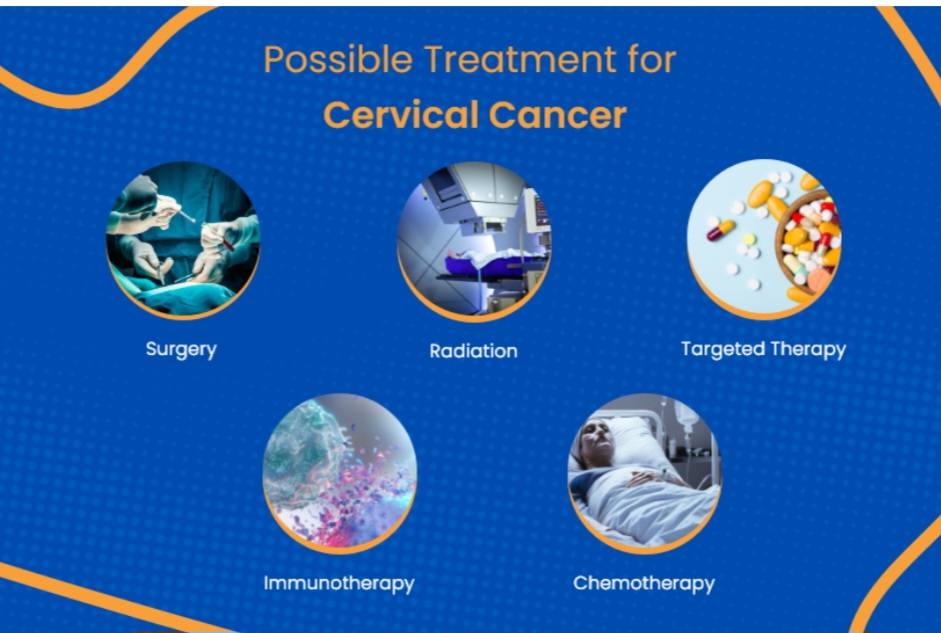
3. Treatment & Medication Safety
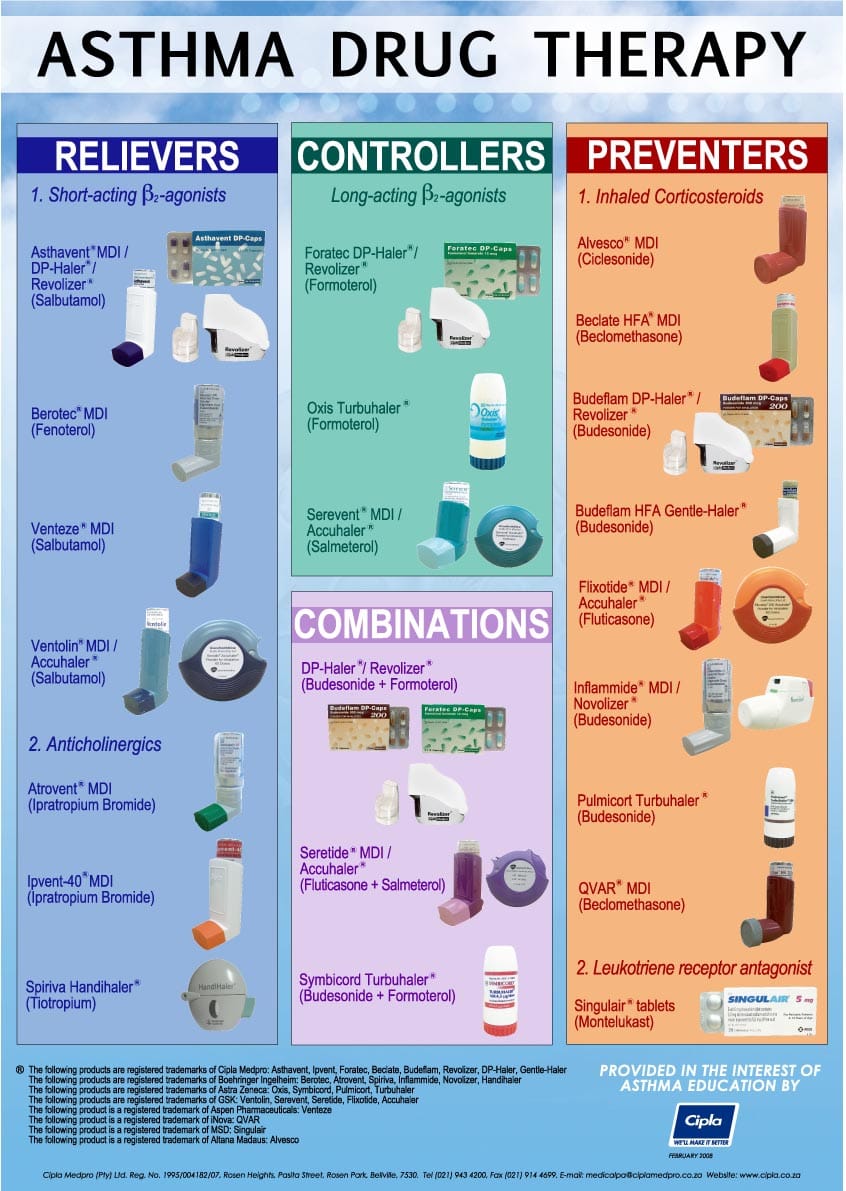
Five Rights of Medication: Right patient, right drug, right dose, right route, right time.
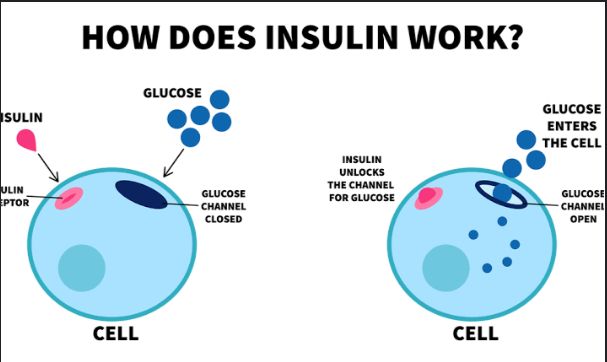
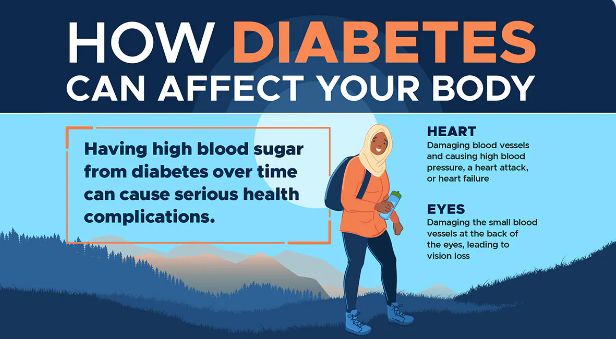
Double-Check High-Risk Medications: Anticoagulants, insulin, and chemotherapy drugs should always be verified by two professionals.
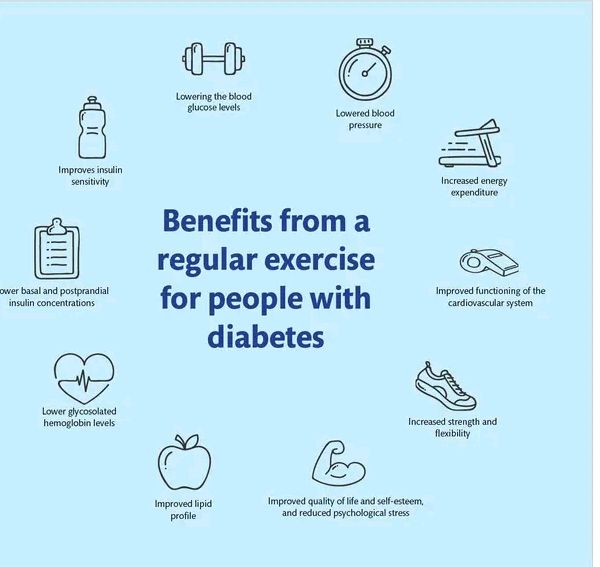
Patient Education: Explain the purpose, dosage, and side effects of prescribed medicines.
4. Surgical & Procedural Safety
WHO Surgical Safety Checklist: Conduct a “time-out” before surgery—confirm patient, procedure, and site.
Sterile Environment : Maintain proper sterilization of instruments and hand hygiene for the entire surgical team.
Team Communication: Encourage open dialogue in the operating room—junior staff must feel empowered to speak up.
5. Inpatient Care & Monitoring
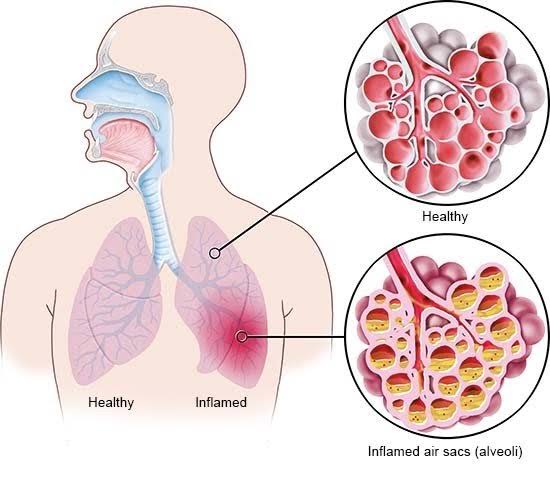
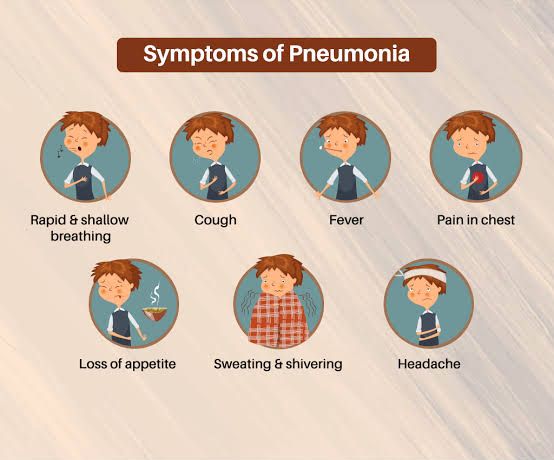
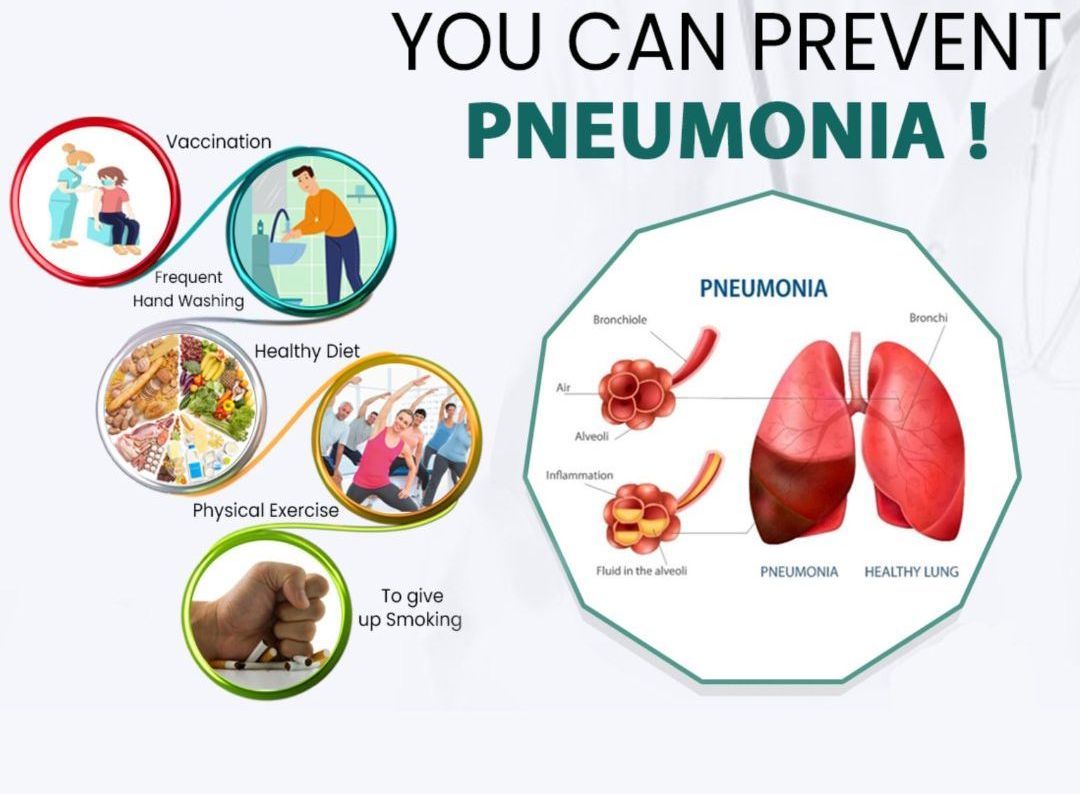
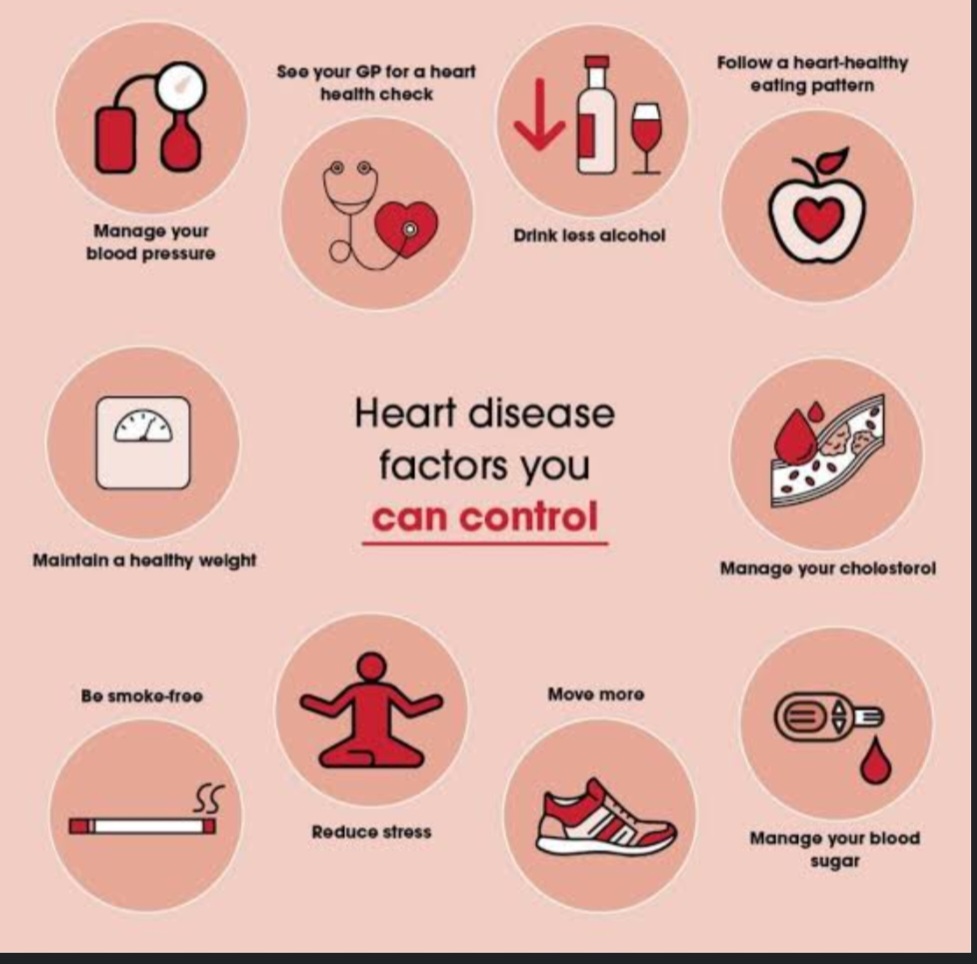
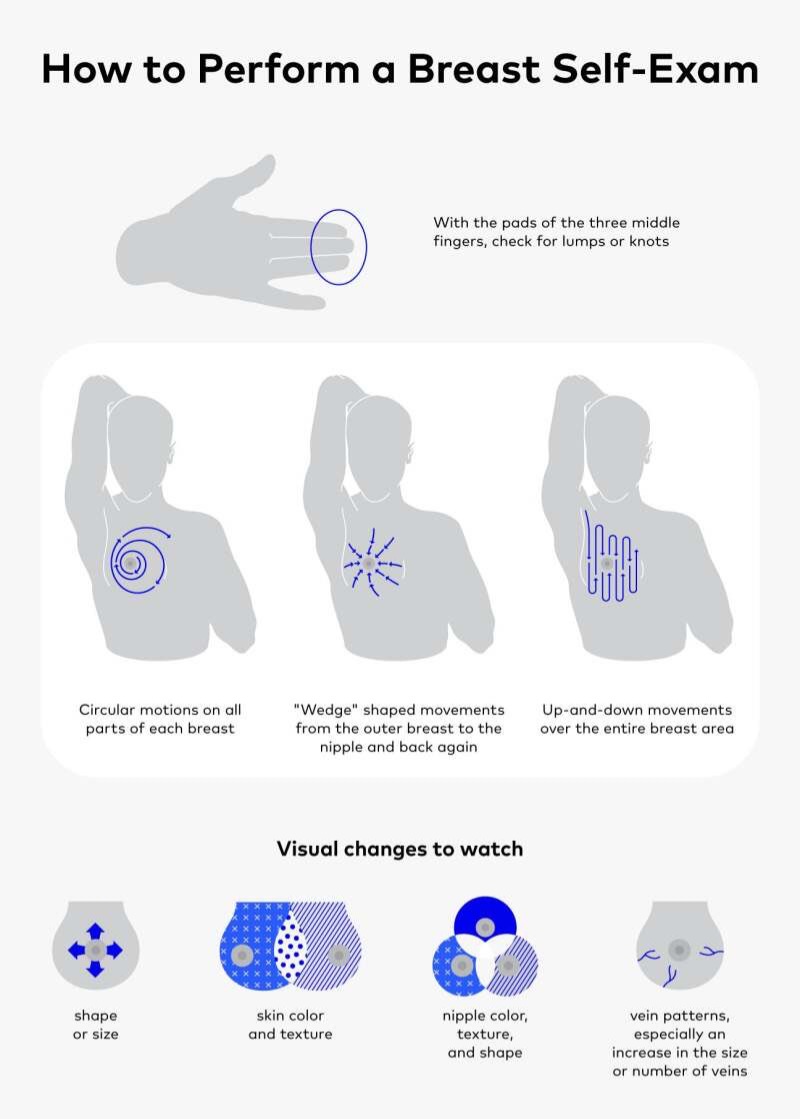
Prevent Infections : Follow strict protocols for catheters, IV lines, and wound care.
Fall Prevention: Keep patient areas clutter-free, ensure adequate lighting, and assist high-risk patients.
Pressure Ulcer Prevention: Reposition immobile patients regularly and use supportive bedding.
Safety Rounds: Conduct daily multidisciplinary safety checks to identify and mitigate risks early.
6. Discharge Planning & Follow-Up
Clear Instructions: Provide written and verbal guidance on medication use, wound care, diet, and activity.
Medication Reconciliation: Review all medicines to avoid duplications or dangerous interactions after discharge.
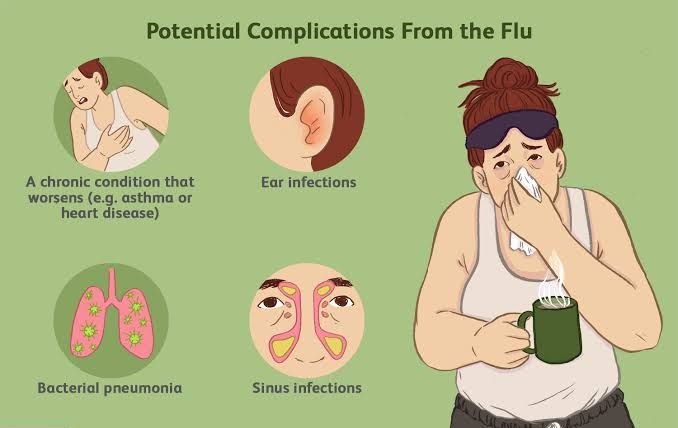
Follow-Up Appointments: Schedule and communicate clearly with patients and families. Missed follow-ups can lead to complications.
Patient Empowerment: Encourage patients to know warning signs that should prompt immediate medical review.
7. Post-Care & Continuous Improvement
Error Reporting: Encourage staff to report near misses and adverse events without fear of blame.
Continuous Training: Provide regular patient safety training for healthcare professionals, including simulations of emergencies.
Feedback Loops: Collect patient feedback on safety concerns and integrate this into quality improvement.
N/B: Patient safety is a journey, not a single action. From the moment a patient enters care, through diagnosis, treatment, recovery, and discharge, each step demands vigilance.