What is Testicular Cancer?
Testicular cancer happens when cells in the testicle grow to form a tumor. It is rare. Majority are germ cell cancers There are two types of germ cell cancers (GCTs)- Seminoma can grow slowly and respond very well to radiation and chemotherapy. Non-seminoma can grow more quickly and can be less responsive to radiation and chemo.
Some testicular cancers do not form in the germ cells i.e. Leydig cell tumors and Sertoli cell tumors.
The type of testicular cancer cell found, symptoms and other factors will help guide your treatment.
Symptoms
At first, the symptom may be hard to notice. The main symptoms of a testicular tumor include:
- A painless lump in the testicle, which is the most common sign
- Swelling of the testicle, with or without pain
- A feeling of weight in the testicles
- A dull ache or pain in the testicle, scrotum or groin
- Tenderness or changes in the male breast tissue
If you find any lump or firm part of the testicle, you should see a doctor to find out if it is a tumor. It should be tested as soon as possible.Â
N/B: Talk with your doctor or urologist if you find a lump that lasts longer than two weeks. The urologist will want to test if cancer is growing or if there’s some other issue, like:
- Epididymitis
- Testicular torsion
- Inguinal hernia
- Hydrocele: when fluid builds up in the scrotum
Causes
It is not always known why cells grow to form a tumor. Also, you may not be able to avoid the risk factors of testicular cancer. The best plan is early detection.Â
Risk factors
- Family history: If your father or brother had testicular cancer.
- Undescended testicles: If your testicles did not drop before birth. This can also be called cryptorchidism and is when a testicle did not drop from the abdomen into the scrotum before birth. A tumor is more likely to grow after this issue.
- GCNIS: These are odd cells in the testicle called germ cell neoplasia in situ (GCNIS) and they are typically found during an infertility test.Â
Diagnosis
Understanding how testicular cancer could affect you starts with a conversation. Your doctor will ask you questions about your general health and talk about your concerns.
Many men are able to identify a problem with their testicles by doing a self-exam. Testicular cancer is one of the most treatable cancers. When caught early, the cure rate is close to 100 percent (where it has not spread past the testicle).
For men with stage II or III testicular cancer, the cure rate is still higher than other cancers.Â
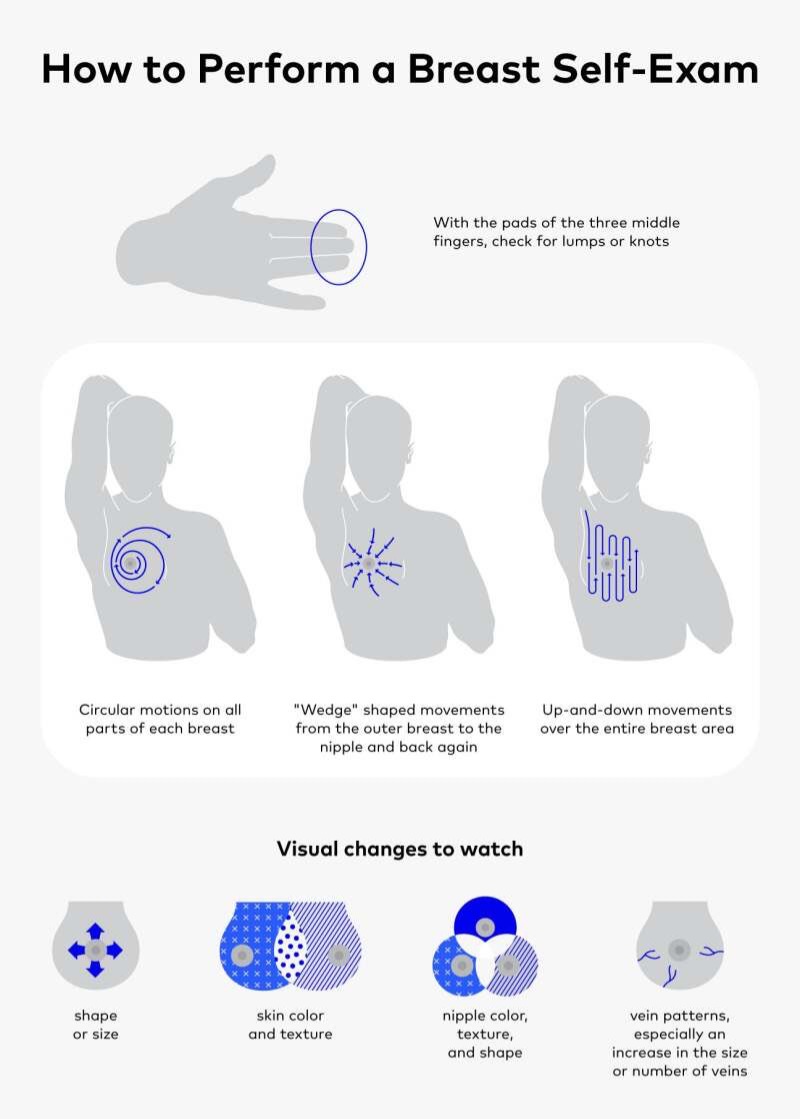
Testicular Self-Exam
The best time to do a monthly testicular self-exam is after a warm bath or shower, while standing, when the scrotum is relaxed. It only takes a few minutes. To start:
- Check each testicle. Gently but firmly roll each testicle between the thumb and forefingers. Feel the whole surface. The firmness of the testis should be the same all around. It’s normal for one testis to be slightly larger than the other.
- Find the epididymis and vas deferens. These are soft tube-like structures above and behind the testicle. These tubes collect and carry sperm. Just become familiar with how these cords feel.
-  Look for lumps, swelling or things that don’t seem right. Lumps or bumps are not normal (even if they cause no pain). Pain is not normal.
- Check yourself at least once per month. Always look for changes in size, shape or texture. If you notice a lump or any changes over time, you should seek medical help. It may be nothing, but if it is testicular cancer, it can spread very quickly.
Medical Exams
Your doctor will talk with you about your symptoms, your overall health and will do a medical exam. If the doctor suspects something is not normal, they will run more tests.
Your urologist will talk with you about your health. They’ll examine your scrotum, belly, lymph nodes and other parts to look for signs of cancer. They’ll look for lumps, firmness or signs of swelling. Tell them if you have a history of undescended testicles.
 Ultrasound
This imaging test is used to see inside the scrotum and check a suspicious lump. Other scans or x-rays may be done if your doctor would like to see inside your chest or abdomen. This is done to see if cancer has spread.
Blood Test
A blood test is taken to check tumor markers. These are proteins and hormones made by some testicular cancers. AFP, ACG and LDH tumor markers rise with some cancers but many testicular cancers will not produce tumor markers.Â
Stages
Testicular Cancer is grouped into the following stages:
- Stage 0: This is also called “Germ Cell Neoplasia In Situ (GCNIS)”. This is not yet cancer, but a warning that cancer could grow. GCNIS may be found in the seminal tubules.
- Stage I (IA, IB, IS): Cancer is found only in the testicle. It has not spread to nearby lymph nodes or anywhere else in the body.
- Stage II (IIA, IIB, IIC): Cancer has spread to one or more lymph nodes in the belly (often the first site of testicular cancer spread). It has not spread to other parts of the body.
- Stage III (IIIA, IIIB, IIIC): Cancer has spread beyond the lymph nodes in the belly. Cancer may be found far away from the testicles, such as distant lymph nodes or the lungs. Tumor marker levels are high.
Treatment
Choices will be based on the exact diagnosis and health of the patient. Before treatment, men should talk with their urologist about whether or not they want to have children. Not being able to have children and changes in male hormones are common after certain treatments. Sperm banking may be useful before treatment, especially if you hope to have children in the future.
Surgery: Surgery is the main treatment for testicular cancer. Based on the diagnosis, other choices may be offered. They may include:Â
- Orchiectomy
- Testis Sparing Surgery
- Retroperitoneal Lymph Node Dissection
- Radiation
- Chemotherapy
Your doctor will always discuss the choice of treatment and the reasons for it.Â
N/B: Beyond basic surgery, care depends on the type of cell and follow-up tests. Even if cancer was found early and treated, follow-up tests are recommended. If, after time, cancer returns, then more treatment will be needed.